Pilot scheme helps improve end of life care in Morecambe

The Integrated Cross-Bay Care Home pilot, between University Hospitals of Morecambe Bay NHS Foundation Trust (UHMBT) and Kendal Integrated Care Community (ICC), has enabled support for a number of residents in residential homes whose wish is to die in their own home rather than in hospital. The pilot involved hospital and community nurses meeting with care home residents, their families and GPs at an informal tea party to have a conversation about what choices are available for end of life care.
The aim was to help individuals make an informed choice about their preferences at the end of their life and agree a plan of care that all parties were comfortable with.
Advertisement
Hide AdAdvertisement
Hide AdFollowing these conversations, over a three month period, there was a reduction in the number of residents admitted to hospital to die.
In Morecambe the number of patients admitted to hospital at the end of their lives reduced from 34 to 16.
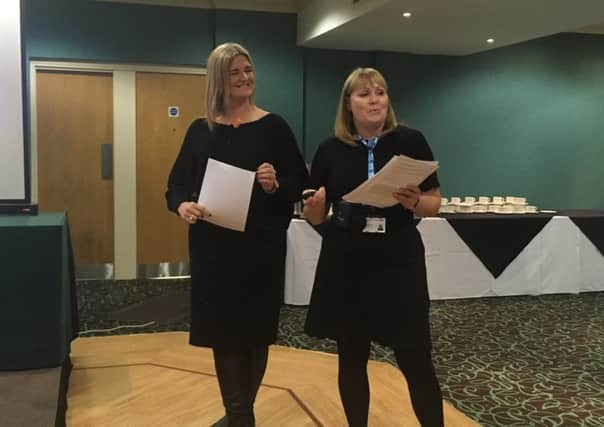
The project, which aimed to ensure that an individual’s wishes were followed when nearing the end of life, was led by Alison Nicholson, the Lead Nurse and Advanced Nurse Practitioner working within the ICC, and Lindsay Pinch, the Bereavement Nurse Specialist at UHMBT, working with three GP practices
The Kendal ICC and the UHMBT bereavement team recognised that between 2014 and 2016 there was a significant increase in the number of patients from residential homes who were dying in hospital.
Advertisement
Hide AdAdvertisement
Hide AdAlison Nicholson said: “There were a significant number of older people coming in to hospital, sometimes three or four a month, having a very short length of stay and then dying. They had actually lived in their care home for months and years and we felt that it would be better for them and their families to remain in their home in surroundings they are comfortable with, wherever possible.”
In Lancaster and Morecambe there are 32 residential homes with 628 available beds (not including nursing home placements).
Alison added: “A lot of it boils down to the education and the support that the residential staff receive when they are trying to deal with someone who is poorly in a care home.
“Nursing homes have nurses, but residential homes don’t so we needed to support these residential homes to help people stay in the homes at the end of their lives rather than send them to hospital.
Advertisement
Hide AdAdvertisement
Hide Ad“We want to work with residents and the families. When you are in a care home it’s best that you plan ahead for example who you want to look after you, where you want to be nursed; those big decisions.”
Lindsay Pinch, Bereavement Nurse at UHMBT, said: “Rather than a formal session, we held a tea party with lots of cake and said, ‘Let’s have a chat, let’s talk about your future plans’ and so many people with different types of illnesses participated.
“Their families came along and participated and at the Morecambe tea party, all the GPs came along as well – it went well with everyone taking on board people’s opinions.
“Sadly there isn’t always a magic wand in hospital, as much as we would love to make people who are at the end of their life better and help them live another five years, we can’t always do that.
Advertisement
Hide AdAdvertisement
Hide Ad“What we can do is to work with families, care home and nursing home staff to ensure that people can choose to die in a their preferred place rather than a busy and unfamiliar hospital environment.”
The success of the scheme has now seen Alison appointed into a joint post working across the local community and within UHMBT to better educate all those involved in providing care at the end of a person’s life.
Following on from the success of the pilot, discussions are taking place with the GPs in the Lancaster ICCs to fund a similar joint nurse post to cover the Lancaster care homes.